
Published August 2021
For years, over a third of Americans have been experiencing sleep deprivation, an issue that’s been exacerbated by stress, grief and anxiety surrounding the pandemic. The sleep crisis has become so prevalent that it has even earned its own term––coronasomnia.
Another growing health concern plaguing the U.S. is dementia, a term used to define the loss of cognitive functioning––caused by damage to the brain cells––in a way that interferes with a person’s everyday life. In the U.S., more than 6 million people live with Alzheimer’s disease, the most common form of dementia, and by 2050 this number is projected to rise to 13 million. While the exact underlying causes of dementia are unknown, experts pinpoint family history, age, head trauma, lifestyle and poor cardiovascular health as risk factors. It has also long been accepted that there exists a connection between sleep and dementia. More recently, new studies have emerged providing deeper insight into the relationship between the two.
Here we’ll explore the connection between sleep and dementia, warning signs you may not be getting enough sleep and how to improve your sleep hygiene.
 Does poor sleep cause dementia?
Does poor sleep cause dementia?
Studies have long questioned the sleep-dementia relationship similar to the chicken-and-egg metaphor. Which comes first––does poor sleep cause dementia, or does dementia cause poor sleep? Research suggests the answer to both questions is yes.
In a long-term study, Harvard Medical School followed 2,800 individuals ages 65 and older. Researchers found that individuals who slept under five hours per night were twice as likely to develop dementia compared to those who slept six to eight hours per night. A different study of nearly 8,000 participants found a 30% increase in dementia risk was associated with sleeping six hours or less at age 50, 60 and 70, compared to a normal sleep duration of seven hours.
Experts are still trying to understand why inadequate sleep increases risk of dementia; however, one theory involves a protein in our brains called beta amyloid. Beta amyloid is the protein that makes up the plaque found in the brains of people with impaired brain function and Alzheimer’s, a neurodegenerative disease. During the day, our brains naturally make this protein. At night when we sleep, our brains flush the protein away. The idea is that insufficient sleep limits the brain’s ability to remove beta amyloid and other substances, causing them to build up until they cause dementia.
 How does dementia affect sleep?
How does dementia affect sleep?
 While poor and insufficient sleep can be risk factors of dementia, sleep problems are also a known symptom of having dementia. Healthy brain function requires healthy sleep, which means our bodies must cycle through the various sleep stages.
While poor and insufficient sleep can be risk factors of dementia, sleep problems are also a known symptom of having dementia. Healthy brain function requires healthy sleep, which means our bodies must cycle through the various sleep stages.
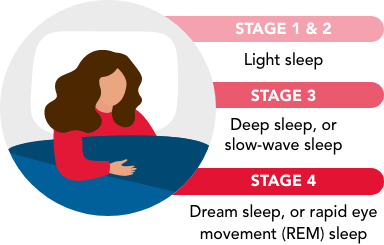
Throughout the night a person can go through four to six sleep cycles that vary in length. During stages 3 and 4, the body restores itself, making these stages essential for cognitive function and overall health. People with dementia spend less time in the later stages of sleep and more time in the earlier stages, which can also worsen as dementia progresses.
Additionally, dementia changes the body’s natural sleep-wake cycle, or circadian rhythm. Individuals who have Alzheimer’s disease often have damaged cells in the brain’s suprachiasmatic nucleus (SCN) and lower cellular activity. Because of this dysfunction, patients are often unable to follow a 24-hour sleep-wake cycle and instead sleep more during the day and less at night.
 How to tell if you’re getting healthy sleep.
How to tell if you’re getting healthy sleep.
Achieving restorative sleep requires a balance of duration, continuity and timing:
Sleep duration: For adults, ages 26-64, experts recommend seven to nine hours of sleep per night, and then seven to eight hours for adults 65 years and older.
Sleep continuity: Since cycling through the stages of sleep into deep sleep and REM sleep are essential to our bodies ability to recover and develop, it’s critical that sleep be continuous and uninterrupted.
Sleep timing: Light and darkness regulate our circadian rhythm, causing chemical reactions in our bodies that either trigger us awake or promote sleep. Misalignment with circadian rhythms can make it difficult to fall asleep, stay asleep and get enough sleep.
Individuals with a healthy sleep pattern will often wake up feeling refreshed and clear-headed, have lots of energy and experience a generally good mood. Meanwhile, if you’re sleep deprived or your sleep quality is poor, you may struggle to wake up, feel irritable, depressed or anxious, struggle to focus or feel tired throughout the day.
 Steps to take if you’re experiencing sleep problems.
Steps to take if you’re experiencing sleep problems.
Poor sleep and sleep disorders can be caused by a number of factors beyond dementia, including lifestyle and mental health issues, such as stress and anxiety and underlying medical conditions. To help reduce the risk of dementia and other health issues, it’s important to understand what could be causing sleep problems and learn how to improve your sleep routine.
- Improve daily routines and habits. For some, sleep troubles are the result of lifestyle choices, such as caffeine or alcohol intake and late-night eating, sleeping environment including lacking the right bedding for comfortable sleep, and pre-bedtime behaviors like bringing phones or tablets to bed. If lifestyle is contributing to poor sleep, implementing new strategies throughout your day and night can help you sleep better. These include designing your bedroom for comfort and relaxation, creating a pre-bedtime, wind-down routine and improving your daily health habits, such as incorporating exercise and making diet changes.
- Take care of your mental health. Sleep and mental and emotional health share a two-way relationship. Not only can sleep problems be a symptom of poor mental health, they can also activate mental health issues in high-risk individuals. In addition to professional therapy and treatment, behavioral health apps can also provide an added layer of emotional support and monitoring. Free or low-cost apps like Calm and Headspace also offer meditations that can help reduce stress and anxiety and achieve more restful sleep. For guided mindfulness sessions led by expert instructors, check out Harvard Pilgrim’s Living Well at Home program.
- Speak to a health professional. If you or a loved one are experiencing persistent or worsening sleep difficulties and find that they’re affecting overall health and safety, it may be time to talk to your doctor. At this time there is no cure for Alzheimer’s or dementia, which is why achieving restful sleep, leading a healthy lifestyle and monitoring your health earlier in life is important for reducing risk of dementia later on.
Take Action: If you are either a Harvard Pilgrim Health Care or Tufts Health Plan member, resources and support related to dementia and overall well-being may be available through your current health insurance coverage. Tufts Health Plan works closely with the Alzheimer’s Association to offer a care management program that helps coordinate dementia care and services for members and their families. Harvard Pilgrim Health Care offers supportive, healthy living programs through their Living Well Everyday well-being program.
To confirm eligibility for any programs or services mentioned in this article as it relates to your specific health plan, please reach out to your account executive or HR benefits team. You may also speak to our member services team at (888)-333-4742 or by sending a secure email. And for plan details and other member resources, log in to the member portal.


